Webinar
Beyond the Clinic Walls: How Telehealth Is Breaking Barriers
Explore the transformative power of telehealth and its future trajectory in our comprehensive webinar. Delve into its remarkable evolution from an emergency response tool during the COVID-19 crisis to a staple in modern healthcare.
Watch on-demand below.
See video policy below.
POST-WEBINAR SUMMARY:
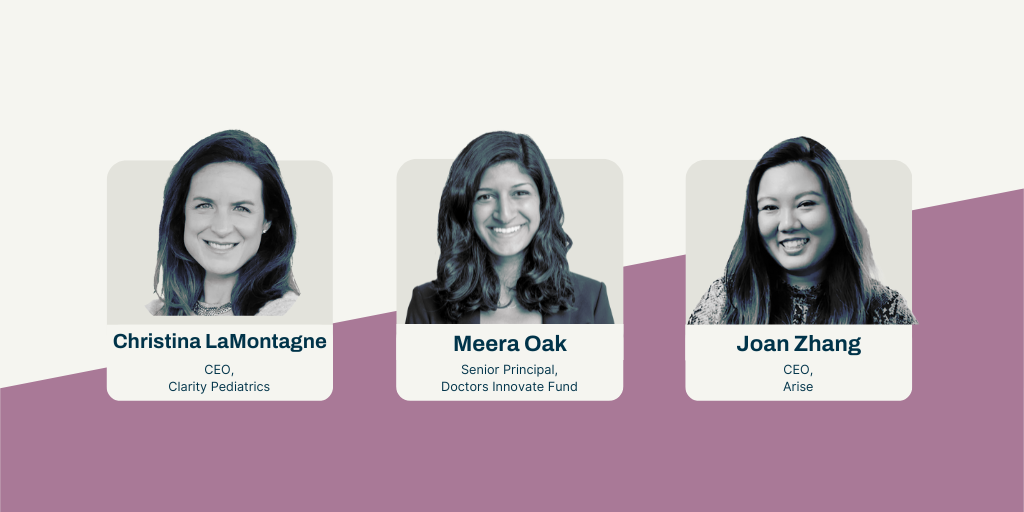
The webinar “Beyond The Clinic Walls: How Telehealth is Breaking Barriers” was hosted by Ludwig Schultz, managing partner at Alumni Ventures. The discussion focused on the growth and potential of telehealth, with insights from Meera Oak, an investment team member at Alumni Ventures, Joan Zhang, co-founder and CEO at Arise Health, and Christina LaMontagne, CEO and co-founder of Clarity Pediatrics. The panelists discussed the benefits of telehealth, including increased accessibility and convenience, as well as the challenges, such as regulatory hurdles and ensuring equitable access. They also highlighted the importance of patient engagement and satisfaction, and the role of data in personalizing care. The webinar concluded with an introduction to the Doctors Innovate Fund, a venture capital fund focused on investing in healthcare startups.
McKinsey’s projection of a surge in telehealth, potentially virtualizing $250 billion of US healthcare spending, underscores its significance. Learn how telehealth has swiftly transitioned from an underused option to an indispensable aspect of healthcare delivery, now anticipated to grow from a $50 billion to a $460 billion market by 2030. This expansion isn’t just impressive—it’s revolutionizing how we approach nonurgent care, mental health, and chronic disease management. Join us to gain insights into this rapidly advancing field, its impact on healthcare, and emerging trends, all hosted by the experts at Alumni Ventures Doctor’s Fund — Meera Oak, Senior Principal, and Ludwig Schulze, Managing Partner.
Our esteemed guest panelists include:
- Christina LaMontagne, CEO of Clarity Pediatrics
- Joan Zhang, CEO of Arise
Why should you watch this webinar? Here are five compelling reasons:
- HomeUnpack the extensive history of telehealth and its definition in the context of modern healthcare.
- HomeDiscover the current technologies and approaches reshaping healthcare delivery through telehealth.
- HomeUnderstand the crucial role of big players in the field, including tech giants and healthcare incumbents.
- HomeLearn about the promising future trends poised to further innovate telehealth services.
- HomeGain expert insights from Alumni Ventures Doctor's Fund Team Members on the investment and development landscape of telehealth.
Don’t miss this opportunity to enhance your understanding and stay ahead in the evolving world of telehealth.
Alumni Ventures is America’s Largest Venture Capital Firm for Individual Investors.
Note: You must be accredited to invest in venture capital. Important disclosure information can be found at av-funds.com/disclosures.
Frequently Asked Questions
FAQ
Speaker 1:
Hi, my name is Ludwig Schultz, Managing Partner here at Alumni Ventures. Thank you for joining us for today’s webinar Beyond The Clinic Walls: How Telehealth is Breaking Barriers. We’re going to slowly get started as everyone settles, and we’ll begin with some of the legal dimensions of the document.So, this presentation is for informational purposes only and is not an offer to buy or sell securities, which are only made pursuant to the formal offering documents for the fund. Please review the important disclosure and the materials provided for the webinar, which you can access at avfunds.com/disclosures, as you see here in the bottom right corner.
Alright, today’s agenda. So, I’m going to give you a little bit of an introduction to Alumni Ventures just for some context. Then we’ll hand it over to Meera to introduce you to our panelists for today, and then I’ll come back and give you a bit more context on the Doctor’s Innovate Fund itself.
So, to begin with a little bit about Alumni Ventures: We are America’s largest venture capital firm for individuals. We serve over 10,000 individual investors today. We have raised capital—over $1.25 billion—and have invested that capital into over 1,300 different portfolio companies.
In essence, you can think about us as having the goal of making venture capital more accessible to more folks—in particular, individuals—which has historically not been possible. We now have over two dozen different funds that we offer every single year and are open to all accredited investors.
In addition, we of course have a larger community of people who are interested to learn about venture capital, to support the individual companies and the founders that are our community—and you’re always welcome to be a part of that as well.
Alright, with that, let me hand it over to Meera for our panel discussion.
Speaker 2:
Wonderful. Hi everyone. My name is Meera Oak, and I’m on the investment team at Alumni Ventures, and today I’m so excited to dive into the meaty topic of telemedicine with two seasoned experts and CEOs from our portfolio: Joan Zong of Arise Health and Christina Lamont of Clarity Pediatrics.Thank you both so much for being here. I want to kick things off maybe with some introductions. I’d love for each of you to introduce yourselves—as I could never do your backgrounds justice—and share a bit more about yourself, but also what you’re building. And maybe Joan, I can start with you.
Speaker 3:
Yeah, sounds great, and so excited to be here to share a little bit more about our perspectives and our work.Briefly, my name’s Joan Zong. I’m based in Houston, Texas. I’m the Co-founder and CEO at Arise, where we’re providing more accessible eating disorder support—that’s done all virtually.
I really come to this work out of my own personal lived experience with an eating disorder that was actually diagnosed when I was in college. And I experienced the barriers firsthand of trying to get care—from the financial barrier of appointments (were hundreds of dollars, even with really great health insurance) to a lot of the just cultural and systemic barriers of—I didn’t have any providers of color on my care team, and ultimately, because of the shortages, no one followed up at the end of the semester.
And so I ended up really just struggling with the eating disorder for more than a decade, ending up in ERs constantly.
And so Arise really came out of my own recovery journey and also the experiences and journeys of the millions of people out there—a lot of the stories that we heard firsthand about how just inaccessible care really is.
9% of the global population has an eating disorder—30 million Americans in their lifetime—yet 90% won’t have access to care. And so really, we’re focused on: how do we solve that problem?
My background is in product, so I am excited to dig into some of the tech side and how do we really innovate and expand access from a technological standpoint. So—super excited to share more.
Speaker 2:
Awesome. Christina, maybe I can hand it to you.Speaker 4:
Certainly. Well, thanks for having me, Meera. It’s such a pleasure to work with you at Alumni Ventures. I’m the CEO and Co-founder of Clarity Pediatrics.I started my career working in HIV and AIDS clinics and really wanting to help underserved populations, and carried that through to my job just before Clarity, where I was working at a large women’s health contraceptive access telehealth provider.
And I’ve always been really motivated by solving for underserved populations and improving the experience of healthcare. And unfortunately, kids are a really vulnerable population within our healthcare ecosystem.
There’s about 75 million kids in the US. Each one of them has family members that are impacted—or their health is in relation to each other—and yet pediatrics is often quite overlooked by the people who pay for healthcare, whether it be the payers or the employers.
And I really wanted to do something about this.
I’d looked at pediatrics in a quite analytic way, and I saw that common chronic conditions like ADHD, obesity, asthma, allergies—the prevalence had about quadrupled since the time I was a kid.
But as a parent, the healthcare system still functions almost exactly the same.
So—who is taking care of the kids, and where is the availability of care, and who’s paying for it—were questions I was really wrestling with.
And so I just wanted to dive into those problems, and that was the genesis of Clarity.
And so we are serving families with kids who have chronic conditions via our telehealth platform. We’re live now in California, but we’re expanding.
And our first indication is ADHD, where—similar to eating disorders—millions of people experience ADHD. About 80% of kids do not have access to the standard of care, but we can make that available through our platform now.
Speaker 2:
Wonderful. Yeah—and so thank you guys so much. Let’s get into this. We have a lot to cover here.To start: telemedicine, or the use of technology to really provide access to remote healthcare services—much like Arise and Clarity are doing—has been around for several decades.
I think we’ve sort of seen it, but I think it truly emerged as this game changer in healthcare in 2020.
And I think that was in part driven by the COVID-19 pandemic.
Pre-pandemic, it was almost hard to imagine how this sort of relatively nascent industry could emerge as this hundred-plus-billion-dollar industry today—and that’s only growing.
Moreover, I think it was really tough to imagine how patients and providers would respond to telemedicine: how the quality of care would be maintained, how the regulatory landscape would respond, and how technology would factor in.
But yet—here we all are, right? It’s 2024, and it’s quite an exciting road ahead.
And so I’d love for you both to maybe take me back to that 2020 era—as builders in the space.
What did you observe during that period, and how did you think about or leverage the adoption that you were seeing?
Speaker 3:
Yeah, I’m happy to jump in here.So I remember pre-2020 at least, there was so much skepticism around whether you could do eating disorder treatment virtually—providers, I think, from everyone around.
And I think 2020 forced us to really try it out and to experiment. And I think what we had seen is—it actually made care a lot more accessible to more people.
I remember when I was going through treatment, one of the big barriers was actually—I had to go to a campus hospital every single day. I had to sit in a public waiting room where all of my peers could potentially figure out that I had an eating disorder.
And so that was a huge barrier to actually continuing with care.
And so I had always thought for many years—telehealth would’ve been such a great solution for that.
What was really beautiful about this transformation over into telehealth is—we see more people getting access to care. Especially our vulnerable populations, like pregnant moms who aren’t able to really take time away from work or from their families to really go to in-person care.
There’s more convenience for Medicaid populations, where maybe, again, they don’t have the time to really go to a physical location for an appointment, and it’s easier for them to maybe—from the convenience of their home—be able to attend their appointment.
So I think we’ve seen expanded access, and I think we’ve also seen that the clinical outcomes—we can still demonstrate really strong outcomes.
We actually—in the eating disorder space—there was a report by FAIR Health that was a spotlight on eating disorder claims. And they saw that the telehealth utilization from 2018 to 2022 increased by over 10,000%, and telehealth was actually the most common place of service for eating disorder treatment in 2022.
So I think it’s—I’m really optimistic about the adoption of virtual eating disorder treatment, and I think it’s done a lot of good for this space.
Speaker 4:
Yeah, I’d love to add to that.Just as Joan is saying in her population—telehealth has been dominant in the last three or four years—I think that’s really true in pediatrics as well.
That convenience factor for parents—a parent or two needing to get out of work, take their kids from school to go to routine appointments—it’s just too much for this population.
And it leads actually to lower outcomes because it’s just so hard to follow through with care.
So I know that the data suggests that telehealth adoption is uneven, and in some areas it’s waning since the pandemic.
But when you’re really focused as a founder on a particular population and their problems, there are these amazing pockets where telehealth is just game-changing.
And I think we really should not go back.
Speaker 2:
You both touched on such strong adoption, especially within your respective patient populations.So I kind of want to stay in that space for a second and just understand how you prioritize patient engagement and satisfaction across your platforms.
You’re founders—you’re juggling a whole slew of different elements of company growth—but obviously the patient engagement and satisfaction is key.
And so I’m trying to understand: what strategies have you found to be most effective in building that patient trust and loyalty?
Speaker 4:
Yeah, I can start this one.We have an approach that really starts with clinical credibility, where—no matter who your stakeholder is in healthcare—a payer, a referring provider, a parent, the patient themselves—everyone wants to be in the right place, with access to a great provider or a great clinic.
And so that’s how we really think about starting that journey.
And we’ve even turned this into one of our company values, where we have to earn trust from everyone.
That’s something that we hold ourselves to day in, day out. So that’s certainly part of it.
I think in our space, time to care—offering a very scarce part of the care ecosystem—has been a big part of it, as well as outcomes.
But really, time to care, access to care—has enabled us to run a lot faster, I think, than if we didn’t have that.
Speaker 4:
And then I’ll just say—we work in pediatrics, which means that a lot of the trust and patient experience that we’re able to attribute is actually through the parents’ eyes. And so we need to think about multiple stakeholders.And to generalize that—because of course not everyone is in pediatrics—I do think that in healthcare it is often complex. Yes, the patient’s point of view is essential as the cornerstone, but there are stakeholders and people that you also need to keep very happy in most business models.
So not forgetting that yes, you need an exceptional user journey with a great defensible product and a killer business model and a great team and all those things, but I think the best founders are thinking more holistically about all the stakeholders within healthcare and whom to prioritize at what times, in what ways—to give themselves that extra edge.
Speaker 3:
Yeah, I love that you referenced your company’s values.Actually, one of the first things that came up for me is—one of our values is “listen to lead.”
And so what that means from a leadership level at our company is listening to our team, but it also has been about listening to our members and their perspectives.
And our model of care—we call person-centered care.
And what that really means is rather than some traditional eating disorder programs that really focus on maybe one modality of care, which might not really be what everyone needs—we actually take the time to listen to each individual’s experiences, their co-occurring conditions, their identities, their past treatment experiences—and really consolidate all of that to really determine the right combination of different types of modalities and therapeutic approaches.
Ultimately, that allows us to deliver better outcomes.
And what we see is that it also really helps members to feel like the care is designed for them, and it’s not like they’re just being fit into this protocol that really often doesn’t account for their needs.
I think a really important second piece is—we have this role on our team called the Care Advocate.
Fundamentally for us, community care is a huge part of our model—really about how do we give folks the tools to really carry forward their healing longer term.
And so this Care Advocate is someone with lived experience with an eating disorder, who’s been in recovery for several years and has had the training to provide the support.
And their whole goal is to really build trust with the member, to really develop empathy with the member and understand what are the social determinants of health that might be at play here, so that we can really better inform our clinical team and staff on how do we make sure that this treatment plan is working for the individual.
And ultimately, we see that because of that Care Advocate, members will stay engaged for much longer.
Because when they have concerns—maybe they lost their job and they’re worried about copays, or maybe just the therapist isn’t the right fit—they have a person that they can really share that information with and they feel heard. And then we can really adapt with the member.
Speaker 2:
Yeah, absolutely. I kind of feel like that sort of segues us nicely into the other side of the equation, which is of course the providers, the Care Advocates, the care team.And I guess—on the same side of the coin here—what strategies are you guys thinking about employing to encourage healthcare providers as they embrace telemedicine, and how they incorporate it into their practice?
Speaker 3:
Yeah, we’ve actually had a lot of providers who are really receptive to telemedicine.And I think being able to work remotely is a huge sell for a lot of providers.
I think one of the things that we really do is take a balanced approach, where we allow providers to do—maybe it’s 30 hours with us and 10 hours they can run their own private practice.
And I think having that split really allows providers to have the benefits of working on a team but also be able to continue their own goals.
So we have a split W-2 and 1099 model, just depending on our needs, depending on the provider’s needs. And I think that flexibility has been really a sell to our providers.
And I think the other piece is really fostering collaboration and camaraderie on the team.
For us, one of the biggest selling points is—you’re getting to work with a cross-disciplinary team of registered dietitians, therapists, psychiatrists, primary care doctors, and peer supporters.
And so, when you’re working in private practice, it’s often just you as a therapist, and you often then have to take on the load of maybe some of the nutrition questions that your client is coming to you with—and you’re not trained in that.
And so being able to work on a team and problem-solve together can be a huge benefit when done correctly and done with the right culture in place.
Speaker 4:
For us—I couldn’t agree more about that clinical camaraderie and support aspect.I think in a startup environment, for many people they can find more of that sense than they found in a more traditional healthcare environment.
So we go out of our way to bring in experts and to support professional development and to get people trained in the cutting-edge new treatment modalities. And I think people enjoy that.
We, as employers, are investing in them in that kind of growth mindset kind of way—a little bit different than other clinics.
We have fewer part-time people—it sounds like that’s something very interesting that Joan has been able to put together for her team.
But what we have done is really ensure that when a clinician comes to us, they become a bona fide ADHD expert.
And so what we try to articulate to candidates is that this is a chance to go really deep in an area that you already care a lot about.
You’re already seeing the need. And when any of us gain mastery—but especially in medicine—higher volumes mean better quality of care.
You’re going to feel this satisfaction because you’re just so good and you’re always honing that craft over and over and over again every day.
And that makes you valuable to the families, but that makes you valuable in your career as well.
And so that again—plus the professional development and the access to other experts—I think has been enticing.
The final thing I’ll say is that many, many providers are burned out. We all know this.
Telehealth companies, I think, have an advantage in that there’s very little crisis and there’s very little call. Everybody does their share, but you can offer often a different work style that takes away some of what’s been soul-crushing to providers in the last five years, but again gives them the expertise and the professional confidence and skillset that comes with a more focused clinical role.
Speaker 2:
Yeah, no—absolutely. And I think you guys sort of framed how you’ve been able to engage again both sides of this ecosystem.And I think “quality of care” really rang true, even when you were talking about the origin stories of your companies.
So I kind of want to spend a little bit of time there—which is sort of understanding, of course, telemedicine’s lauded for the potential for increased patient engagement and experience.
And clearly you guys are finding that within your respective companies.
But I just want to understand—how do you maintain and monitor that quality of care when it’s delivered through telemedicine?
And are there metrics, are there benchmarks that you’re using to assess effectiveness in these services?
Speaker 4:
All the metrics you stated do matter. I’ll add time to care, and then short- and long-term clinical outcomes as well.But there are many things that are important in quality—not just one measure.
I’ve been very fortunate, as the business co-founder, to team up with a clinical co-founder and have very strong clinicians across my team.
And I really credit them in understanding how to set up safety, quality control, compliance.
We also had great legal input, but as a team that really built the policies, it makes it happen every day.
So we do carve out time in different schedules for safety and compliance as well as quality control. And it’s just a daily devotion.
It’s back to values and culture—it just has to be part and parcel of what you do, top to bottom and bottom to top.
Every patient has to matter.
And so again, for us, I think there’s lots of frameworks and best practices I could articulate, but it really was the DNA of my co-founder and early clinical experts that I think has led to a best-in-class quality and compliance system.
And then just never stopping. New things are going to come up all the time. You’re going to expand your clinical program.
And the risk is obviously huge when you’re in healthcare.
So we take that really seriously. And I think I’ve had enough experience in my career to know that things can and will go wrong, and it’s really scary when those things happen.
So you feel very intrinsically motivated to avoid every risk you can.
Speaker 3:
Yeah. Christina, I love that you have such a strong clinical leadership team.And I think that’s one of the things that I really want to just highlight—there are so many startups out there where clinical leadership is really not at the forefront, and it’s really showing.
And it’s really, I think, a stain—I think on a lot of our reputations—when that happens.
So I think it’s been so important for us as well to really center clinical leadership and experience.
And I think what’s really important is finding a clinical leader who is values-aligned and also has a little bit more flexibility.
I think all clinicians are not the same. Some are a lot more protocolized and a little bit more rigid, and some see some of the gaps in their existing treatment models and see the opportunity to really innovate.
And so our Chief Medical Officer, Dr. Erica Taylor, is truly incredible in that way.
And I remember—we just have conversations around how she’s always done things, but there’s opportunity to improve on that.
Because we’ve seen that if 90% of people are not getting care—that’s an issue.
And so for us, it really comes back again to person-centered care.
And so what we really do is—we have defined eating disorder measures that we’re certainly looking at, like the EDE-QS is a main measure.
We also look at mental health benchmarks like the PHQ-9, GAD-7.
We look at quality of life, as well as time to care.
And for us, what’s important too is our ability to prevent escalation into hospitalization again.
So those are all really important. But longer-term, for us, what’s really important is that a member understands what these metrics are and what these benchmarks are—so that way, longer-term, they can really carry forward that healing for themselves.
Speaker 3:
So what we really try to do is—from the very beginning, as we’re developing that treatment plan—we will tell them, “Here’s what an EDE-QS is.”It’s the Eating Disorder Examination Questionnaire. It’s a 12-question questionnaire that really goes through eating disorder symptom frequency and severity.
And we will kind of check in every appointment on how you’re progressing. And we show them a chart on how things are trending, and that way they have that knowledge of, “Okay, this is why you’re asking me all these questions every time. And I can use this longer term as a check-in just for myself to see how I’m doing with the eating disorder and the progression.”
I think one of the most exciting moments was when a member of ours mentioned to their Care Advocate during an appointment—
Hey, they asked the member, “What was the highlight of your week?”And the member said, “Well, I saw that my EDE-QS score dropped significantly over the past few months, and I just really am so proud of myself for that.”
And I think that seeing that progress is so key, I think, in the mental health space, where oftentimes it just feels like things are often feeling like they get worse before they get better.
And so having something to really benchmark your progress—and to see the progress that you’re making—is so, so important.
I think with physical health, we see—let’s say A1C levels or glucose levels—you see the trends moving in the right direction. And I think we need something like that in the mental health field and especially for eating disorders, for people to feel a sense of progress to continue.
Speaker 5:
Let’s take a quick time-out to tell you a bit about Alumni Ventures and our Doctors Innovate Fund.AV offers the opportunity for individuals to invest in startups shaping the future.
We build diversified portfolios co-investing alongside renowned lead investors. Today we serve over 10,000 investors who have invested over $1.3 billion.
With our Doctors Innovate Fund, you’ll have the opportunity to invest in a portfolio of 15 to 20 tech companies founded by entrepreneurs and doctors—from transformative healthcare services to groundbreaking diagnostics.
Our founders are paving the way for a healthier tomorrow.
So if you’re interested in making a meaningful impact and helping to drive the next wave of medical breakthroughs, visit av.vc/doctors.
Back to the presentation.
Speaker 2:
I want to turn the page a little bit and think about expansion with telehealth services.And of course, what goes hand in hand with telehealth expansion is always regulation and regulatory hurdles.
And so I am sure each of you can sort of touch on this, but I would love to understand:
What are the most significant regulatory challenges for telemedicine—or for your specific companies—as you think about expanding into different regions, and how did you navigate those complexities?
Speaker 3:
Yeah, this is a great question.So we’re currently in Texas and North Carolina, about to expand to New York and Florida. And this has been just the standard challenge from every single digital health company that I’ve been at—is our ability to expand to new states.
Because it feels like, honestly, we’re dealing with 50 different countries.
And there are some little pieces here and there that make it a little easier, like the medical compacts, the PSYPACT—but at the same time, it still just is such a significant challenge to really get ready in every state, to get your providers.
And it’s also really expensive.
And so we’ve taken more of the approach of: go really deep in markets, go really local, and really become part of the community—get to know some of the referring providers, know the referring community organizations.
And I think we will continue to really take that, but at the same time—we get hundreds of people reaching out and saying, “Hey, do you have services in this state?”
And it’s like, “Well, we will be soon.” But right now, from a regulatory standpoint, we really just can’t. Our providers legally cannot.
And so if I had a magic wand, it would really just be to standardize this process.
And I want to say too—it’s not even just, “Oh, all 50 states have different rules and regulations.” It’s also different rules and regulations for every single different type of specialty.
So for us, it’s like—even within just the category of therapist—LPCs versus LCSWs versus psychologists—it’s all different.
There’s a whole team that you have to have in place to just really know what you’re getting yourself into.
You have to forecast almost like a year out sometimes for some states you’re going to launch next year, and it just becomes really an operational nightmare.
And I think the second piece on regulatory is—I think there’s a lot of opportunity to innovate with Medicaid.
And I think I’m most excited about ways that we can start to expedite that process.
It takes a long time to get providers enrolled and credentialed, and I think there’s opportunity for us to speed up that process so we can get these much-needed resources to these communities.
Speaker 4:
I think Joan brought up so many good points that I just want to plus-one across the board.Maybe I’ll start where she left off.
We have secured Medicaid contracts now for several counties in California, and it took a long time.
And back to all the things we’ve been talking about—you’re trying to scale great access to high-quality care, and it often feels like the system is just working against you.
It’s just very hard to make the moves that you think your patients deserve.
Not to mention the costs, and the operational headaches, and the forecasting challenge as a one-and-a-half-year-old company—that you just articulated.
I would say on top of that—and on top of being a founder—I’m also an angel or an advisor to about a dozen other companies in this space.
Everybody’s got a problem or a risk that they’re taking somewhere or other—whether it be prescribing risk, or async versus sync visits (and different states have different rules), reimbursement risk, CMS risk.
We are working in a disease where the standard of care requires a controlled substance. And there are different ways, of course, that those substances need to be managed.
But again, there’s federal ambiguity on multiple levels about how these drugs will be managed in the future—not to mention all the ambiguity that comes on different levels at the state level.
So I just see across the board that it can feel really hard to expand access quickly.
And to your point about magic wand—nobody enters, nobody takes on the risks and throws themself into being a founder to hit legal roadblocks to do the thing that every doctor is telling them should be done.
And you used a great word—how do we expedite? How can we do things faster?
There’s always hope, but I just wish that there were more systematic ways of doing that at times.
I’ll also just add that depending on your business model, you may feel these pressures more or less.
There are many business models where being in 50 states is really important right off the bat—because your business model is direct-to-employer or whatever it might be.
And there are workarounds for that, but even then, you’re taking on a different type of risk—maybe—than what Joan’s and my business looks like, where we’re going deep in particular markets.
So there are now tried-and-true ways of working through the complexity, which is great—we don’t have to make it up as we go in the way that our peers 10 years ago did.
But it still feels hard.
Speaker 2:
Yeah, no, absolutely. And I feel like this sort of lends itself nicely into the next area I wanted to talk about, which is accessibility.And I think at times, expansion—this sort of promise of telehealth, its ability to reduce cost, to break these geographical barriers—there’s so much promise here.
But I think that there are still challenges when it comes to accessibility.
And that’s the question I pose to both of you: how do you think about ensuring equitable access to telehealth services?
It’s sort of breaking down one barrier, but are there many to go? I guess that’s my question for you.
Speaker 4:
Yeah, what comes immediately to mind is something near and dear to my heart.So my co-founder is a Guatemalan immigrant, and it’s just been very important to us from day one—especially in a place like California—that we offer culturally sensitive, multi-language care to different populations.
I think what’s really hard though, as an early stage company, is you’re trying to evolve and change and iterate on so many things at once so quickly.
And then to also be making the time and the intention to interpret—or better yet, the things you learn in serving some populations—you bring back to other populations.
But it’s just that things are moving quickly, you’re iterating quickly, and trying to figure out how to keep up across all the dimensions that you care about.
We just started in Medicaid, we just started in Spanish. But then there are other forms of equity.
For us, again, we really encourage two parents to attend care on behalf of their children, but sometimes that’s not possible, or there’s a non-traditional family structure.
And we think a lot about what does equity mean when what’s best for the child is both parents and care people are there, but again, the traditional system isn’t quite set up for that.
So how do we cross the chasm from an equity point of view?
So again, I think every business is a little bit different, but understanding your user and what matters most to them is a good place to start.
Speaker 3:
And actually, Christina, I’m really just glad that you brought that point up because I actually have a dear family member who was not able to get treatment for ADHD or even get the diagnosis because there was a lot of stigma in their family around mental health and just denial that there was anything wrong.And it wasn’t until they were an adult that they were finally able to even start that process for themselves.
And even then, it required that they get their parents to give them kind of a report on what they were like growing up.
And they’re like, “I can’t do that.”
And so thankfully, I was able to step in and provide some of that background and history.
But I think to your point, we need to be thinking about some of these access barriers that people will have.
I think for us on the eating disorder side, there are two really big categories.
One is still financial barriers.
I mean, there are a ton of programs that have moved into the virtual space, but they’ve effectively just taken their care model that they had—that was already inaccessible—and just made it virtual, at the same price point or barely a discounted price point.
Sometimes for eating disorder treatments, it’s like $15,000 out of pocket for people for a couple months of care—which I know I couldn’t afford.
And so I think first of all, it’s really thinking financially about how do we make this care still work from a cost perspective for a business, but then also be more accessible to the people who need it the most.
And so for us, similarly, we’ve really prioritized getting our providers enrolled with Medicaid and really focusing on Medicaid populations.
So that is one piece: how do we really partner with health plans to be able to pay for these services and make it more affordable?
But then on the flip side, to Christina’s point on the cultural side and some of the other access barriers—just because it’s affordable doesn’t mean the care model also has to work.
And so to your point, I think a lot of eating disorder treatment, especially when it’s for young teens and children, there’s a common model—FBT, family-based treatment—and it requires, again, that you have a parent or caregiver who can really monitor your entire treatment.
It requires a significant amount of time.
And so when you think about Medicaid populations where maybe the parent isn’t even involved—maybe this is a kid in the foster care system—or maybe that parent is working a handful of jobs and doesn’t have the time.
Or even—I talked to someone who’s in the VC space who had a kid with an eating disorder and just doesn’t have the time.
And so we need to really be thinking about alternatives where we provide more flexibility.
And it doesn’t have to be maybe the 15 hours a week of required clinical time.
If someone only has two hours to give—let’s not just turn them away. Let’s try to get them the most important care that they need to really prevent them from getting worse.
And I think for us, that flexibility has been so critical to really make sure that people can just start the care process with us.
Speaker 2:
I feel like we could drill into so many more topics on this call—and this is amazing—but I want to maybe end on a bit more of a forward-looking question.We’re in this era of—every single day there’s a new technological innovation: AI, IoMT, 5G.
There are so many new technologies emerging, and I’m just curious to hear:
Where are some of the most exciting technologies you are seeing in your space particularly, and then are you doing any work to incorporate them or plan for them as you look out over the next five years or so?
Speaker 3:
Yeah, I can kick us off with this.So my background’s in product and tech, and this is what I really love doing.
And I was previously at Headspace—so just love the consumer kind of tech side of everything.
For me, I think one of the most important pieces is: how do we actually use data to better personalize care and actually get closer to developing more N-of-one care models?
What I mean by that is—rather than every single person following the same treatment protocol—how do we use more of our predictive abilities to say,
“Hey, the right dosage—so to speak—of care appointments is this.”
Or, “The right provider match is this person.”
“The right therapeutic approaches are a combination of these pieces.”
So that way, we really think that we’re optimizing for each individual’s prognosis and treatment success—rather than just kind of trying to fit everyone in the same model.
And so what we’re trying to do now is—as we’re really building up our patient cohort—really start to learn what are some of the patterns that we’re seeing, the correlations that are leading to better outcomes, and start to build models to really better predict that.
I think the other piece that I’m really excited about is creating more consolidation and just connectivity between systems—and starting to work towards some even just digital biomarkers for eating disorder care—where we can better sense like,
“Oh, based on some of these factors that we’re seeing—maybe if it’s just your activity level has changed or your sleeping patterns have changed or things like that—we can actually determine:
‘Hey, maybe it’s time to go check in with your therapist briefly.’”
Things like that where it doesn’t require the member to have to self-report—something that we can gauge in their day-to-day.
Speaker 4:
Yeah, great points.In a phrase, we think about how we can bring precision medicine to what is today more of a behavioral health realm.
So some of the things that you might do in cardiology—what my co-founder does to ensure great outcomes—how do we use some of those same types of analytics and measurement across healthcare more generally?
So it’s things like user journey, things like matching.
But then also—not everyone learns or absorbs medical information in the same way.
And then fundamentally, if the basis of our business is there’s not enough supply of pediatric specialists—how do we do everything from reorganize their day to really enable much more automation in the way that care is delivered, in the right way for the right person?
And so that it feels very much more like precision in terms of who the person is—as Joan was saying—and also in terms of being able to predict what the outcome would be from that very precise intervention.
Speaker 2:
Fantastic. I want to thank you both for taking the time to be with us today. I think that’s all the time we have, unfortunately, but I really appreciate it.And with that, I will hand it back to Ludwig. Thank you, guys.
Speaker 1:
Thank you, Meera, so much for that introduction and the panel on telehealth.Very much appreciated to have Christina and Joan join us today and share their insights about what it takes to build a business in telehealth and medicine.
So with that piece of the panel concluded, we’re going to turn our attention to an introduction to the Doctors Innovate Fund itself.
So that’s exactly the fund that Meera and I and the rest of our team work on together within the context of Alumni Ventures.
So what is the Doctors Innovate Fund?
It is, very simply, a fund focused on solving healthcare problems by investing into venture-backed businesses.
Some of those businesses will have doctors as founders, some of them will have entrepreneurs who are seeking to solve healthcare problems.
In all, the fund will have somewhere between 15 and 20 companies that we invest into on your behalf.
Those companies will be diversified by stage, by sub-sector, and by lead investors—which I’m going to touch on a little bit more in a moment.
These funds are available to you to invest in starting at $50,000—but of course, all the way up into the millions as well.
There are opportunities for fee discounts at levels above half a million dollars, a Diamond Club that we’re happy to give you more information about, and also important implications for tax and the option of investing via retirement funds.
So there’s lots more information that you can learn about in those practical dimensions.
A bit about how we identify and how we evaluate the opportunities.
So the Doctors Innovate team—my team, Meera, myself, and the rest of the team—are part of a larger group, Alumni Ventures, of which we are 40 investment professionals across the United States in major markets.
We are evaluating and identifying investment opportunities together. We are then investing into those opportunities together and ultimately building these portfolios on your behalf.
As I mentioned before, and perhaps one of the more important parts about how we invest, is that we’re never the first or the only investor into a company. We are investing alongside other established venture capital funds like these that you see here. These are funds who have a long track record, a long history of investing into venture capital, a lot of expertise, and we benefit from all those pieces when we invest with them. Certainly do not want to be competing with these folks given their expertise and their knowledge.
This fund will be built up with a lot of different subsegments in health tech. So these are just a few examples—not necessarily that we’re going to hit all of them—but you can imagine there’s plenty to be done in insurance and payments. There’s lots of opportunities for health and wellness and prevention, education, clinical trial enablement, et cetera. Lots of opportunities ultimately in healthcare, and we’re going to seek to have a variety. And telehealth, of course, will be a part of these, but it won’t be the only thing that we do in the Doctors Innovate. We’re going to have a variety of different areas that we invest into.
A couple of examples of companies that we’ve historically invested into with Alumni Ventures that would fit within the Doctors Innovate mandate: the easy one that I love to point out is the Oura Ring that I wear every day. This is a smart ring—think about it as providing all the same information as an Apple Watch and obviously in an interface that is pretty straightforward and simple to carry around.
Another example we have here is Precision Neuroscience. I’m sure you’ve heard of Neuralink, one of Elon Musk’s many companies. It turns out that Elon created Neuralink with a bunch of other founders. Some of those founders decided to leave and created an independent new company, and that is Precision Neuroscience. We’ve been investors in Precision for a while, and they’re doing amazing things in the brain-computer interface.
Strongly encourage you—take a look at these websites: Precision Neuro, SonderMind, Oura, Kindbody, Iris Plans. These will give you an example of the type of companies that we’ll be investing in on your behalf for Doctors Innovate.
Now, some practicalities. There are some deadlines and some discounts. Unfortunately, as of the recording time for this event, you’ve missed the first deadline, but there is still a second deadline at the end of March, which will provide a 5% discount on the management fee. And ultimately, you need to make a decision if you’d like to join us this year by April 30th.
And I’ll point out that these are signature deadlines, not funding deadlines. Funding can occur subsequently.
If any of this is of interest—if you’d like to learn more—a couple of different ways that you can do so. One is to go to av.vc/doctors. This will lead you to our data room. You can read up on the fund, how we approach things, and more about all of the dimensions that need to be considered in joining us for an investment. As well, in there you can find an opportunity to schedule time with Stacy or one of our other senior partners to speak one-on-one with her about the opportunity and any questions that may be specific to you.
Otherwise, you’re welcome to email us at [email protected]—ask any questions there. That’ll go to our investor relations folks, and they can help you with any practical matters along the way.
So thank you again so much for joining us today. I hope you found this panel of interest, and we’ll look forward to continuing the conversation with you in future.
About your presenters

Partner, Healthtech Fund
Meera’s background includes strategic, financial, and operational experience from her time at Yale University, where she managed a $1B budget (of a $4B organization), led M&A transactions, and secured business development relationships with corporate partners. Most recently, she worked with early-stage venture funds and incubators like Create Venture Studio and Polymath Capital Partners and was responsible for launching business ventures and sourcing investments in enterprise SaaS, infrastructure, and ecommerce. Meera has a BA in Economics from Swarthmore College and an MBA from the Tuck School of Business at Dartmouth.

CEO, Clarity Pediatrics
Health technology leader with experience across operations, innovation, investing, and M&A. Two-time executive at high growth, venture-backed start-ups achieving >$100M ARR and profitability: Pill Club and NerdWallet (NASDAQ: NRDS). Previously a Corporate Development executive at J&J. Excited about building teams, transforming patient experiences, and finding data-driven approaches to improve health outcomes.
Aims to accelerate the impact of technology across the healthcare sector. Angel invests in exceptional founders, advise early-stage companies, partners with VCs to deploy smart capital, and develops and attracts breakthrough talent.

CEO, Arise
Joan co-founded Arise out of her own lived experience with eating disorders and mental health conditions — and deep empathy for the diversity of mental health journeys of so many others that drives her work as a product leader in the mental health tech space. Prior to founding Arise, Joan was a senior product manager at Headspace Health where she led initiatives that empowered members to get into clinical care faster than ever. Prior to Headspace, she was a lead product manager at Click Therapeutics developing a digital treatment for major depressive disorder. Joan started her career in management consulting at Deloitte where she led projects to implement robotics process automation at a top global pharmaceutical company and EHR systems for a state-wide development disability service provider.